Thoracentesis
- Home
- Services
- Pulmonology
- Thoracentesis
What is Thoracentesis?
Thoracentesis is a medical procedure used to diagnose and treat certain conditions affecting the lungs and pleural space. The procedure involves the insertion of a needle through the chest wall into the pleural space to remove excess fluid or air. It is commonly performed by pulmonologists, thoracic surgeons, or interventional radiologists under sterile conditions.
What is the importance of understanding the Pleural Space?
Before delving into thoracentesis, it's crucial to understand the anatomy of the pleural space. The pleura is a thin membrane that lines the lungs and the inside of the chest cavity. Normally, a small amount of fluid is present in the pleural space, allowing the lungs to expand and contract smoothly during breathing. However, certain medical conditions can lead to an abnormal accumulation of fluid (pleural effusion) or air (pneumothorax) in this space, which can cause breathing difficulties and other complications.
What are the indications for performing Thoracentesis?
Thoracentesis may be performed for both diagnostic and therapeutic purposes
Diagnostic Thoracentesis
Identifying the Cause
It helps determine the underlying cause of pleural effusion or pneumothorax. Common causes include infections (such as pneumonia or tuberculosis), congestive heart failure, cancer, or autoimmune diseases.
Fluid Analysis
The removed fluid is sent to a laboratory for analysis. This can reveal important information such as the presence of infection, cancer cells, or signs of inflammation, guiding further treatment decisions.
Therapeutic Thoracentesis
Symptom Relief
Removing excess fluid or air can alleviate symptoms like shortness of breath or chest pain, improving the patient's comfort and breathing capacity
Treatment of Recurrent Effusions
For patients with recurrent pleural effusions, thoracentesis may be performed regularly to manage symptoms and prevent complications
How Thoracentesis is Performed?
The procedure is typically performed in a hospital setting or outpatient clinic. Here’s a step-by-step overview
Preparation
The patient is positioned either sitting upright or lying down on their side, depending on the location of the fluid accumulation. The skin over the chest area is cleaned and numbed with a local anesthetic
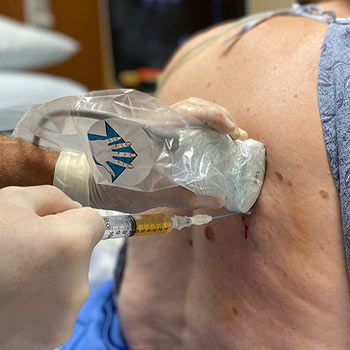
Insertion of Needle
Using ultrasound guidance for accuracy, a needle is inserted through the chest wall into the pleural space. In some cases, a small incision may be made to facilitate the insertion of a catheter
Fluid or Air Removal
Once the needle or catheter is in place, the excess fluid or air is withdrawn using a syringe or suction device. The amount removed depends on the patient's condition and symptoms.
Monitoring
Throughout the procedure, the healthcare provider monitors the patient's vital signs and symptoms for any signs of complications, such as pneumothorax or bleeding.
Post-Procedure Care
After the fluid or air is removed, a dressing may be applied over the insertion site. Patients are often monitored for a short period to ensure stability before discharge.
What are the risks and complications associated with this procedure?
While thoracentesis is generally considered safe, it carries some risks, including
- Pneumothorax: Accidental puncture of the lung tissue can lead to air leakage into the pleural space.
- Bleeding: In rare cases, the procedure may cause bleeding around the puncture site or into the pleural space
- Infection: Although rare, there is a small risk of introducing infection during the procedure
How should patients be monitored post-thoracentesis?
Most patients experience immediate relief of symptoms after thoracentesis. However, it's important to follow any specific post-procedure instructions provided by the healthcare team. This may include avoiding strenuous activities for a short period and monitoring for any signs of complications, such as fever or worsening breathing difficulties.
Thoracentesis is a valuable procedure in the field of pulmonology, offering both diagnostic insights and therapeutic benefits for patients with pleural effusions or pneumothorax. By safely removing excess fluid or air from the pleural space, healthcare providers can improve patient comfort, diagnose underlying conditions, and guide further treatment strategies effectively.
